In January 2026, the U.S. Departments of Agriculture (USDA) and Health and Human Services (HHS) released the 2025–2030 Dietary Guidelines for Americans. These guidelines shape national nutrition policy and influence everything from healthcare recommendations and senior nutrition programs to how communities think about food, aging, and long-term health.
Updated every five years, this edition represents one of the most meaningful shifts in federal nutrition guidance in decades. Rather than focusing narrowly on calorie reduction or individual nutrients, the new guidelines reflect a growing body of evidence centered on food quality, metabolic health, functional aging, and disease prevention.
For older adults in particular, these changes are both timely and long overdue.
A Shift Toward Food Quality and Function
Previous dietary guidance often emphasized eating less, avoiding fat, and limiting calories. While well-intentioned, this approach frequently overlooked how aging bodies actually function.
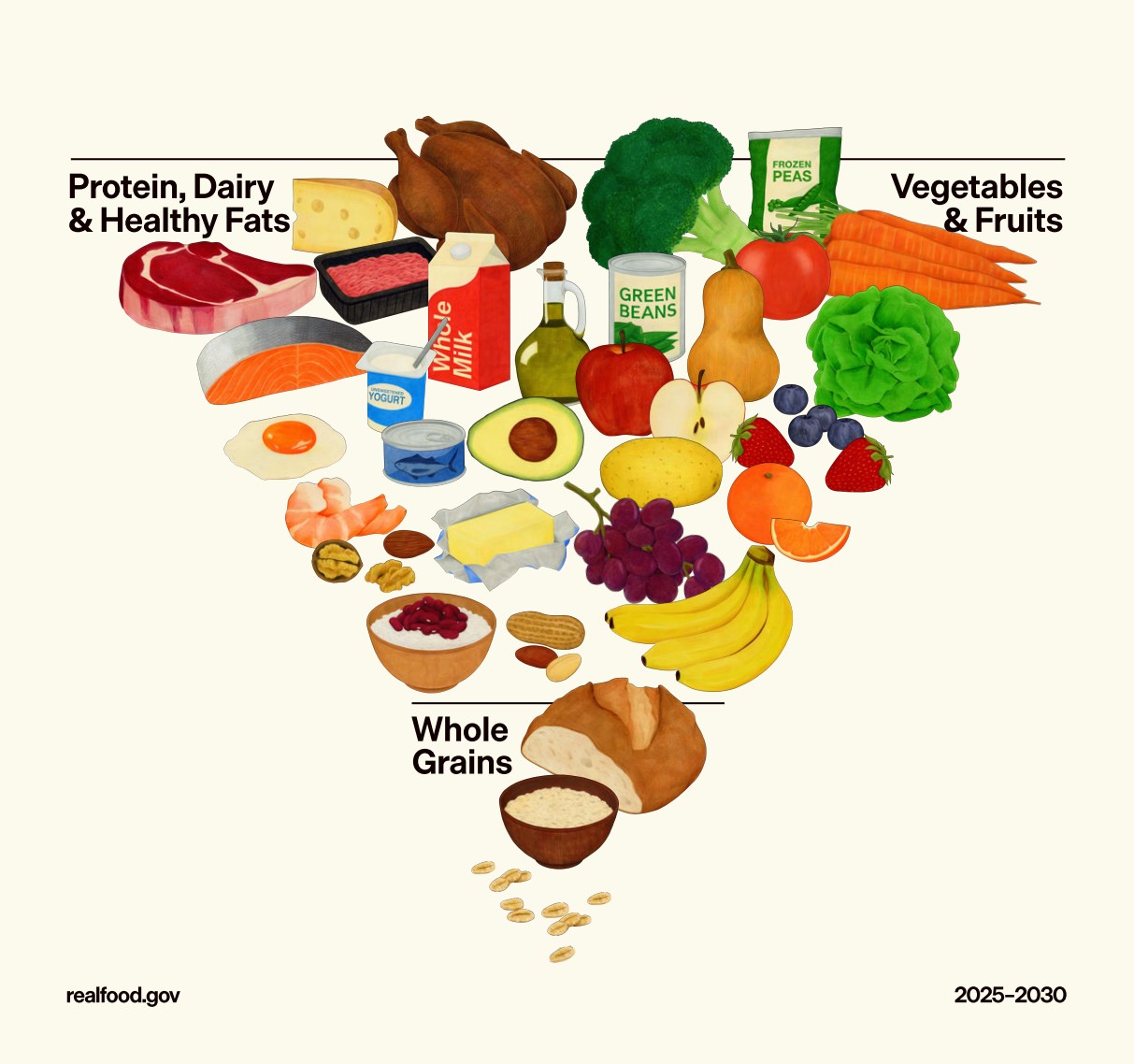
The new guidelines signal a shift toward dietary patterns that support strength, resilience, and long-term health. They emphasize whole foods, nutrient density, and metabolic stability rather than restriction for its own sake. This reframing is especially important for older adults, who often eat fewer calories overall but have higher needs for protein, micronutrients, and energy quality.
Protein Takes Center Stage
One of the most significant updates is the stronger emphasis on protein intake.
The guidelines now recommend consuming high-quality, nutrient-dense protein at each meal, with intake targets ranging from approximately 1.2 to 1.6 grams per kilogram of body weight per day. This represents a meaningful departure from the long-standing minimum recommendation of 0.8 g/kg, which was designed to prevent deficiency rather than support optimal function.
For older adults, adequate protein intake is critical for preserving muscle mass, strength, balance, and independence. Progressive aging research has consistently shown that higher protein intake, especially when evenly distributed across meals, helps counteract sarcopenia and reduces the risk of falls, frailty, and prolonged recovery after illness.
Rethinking Fat and Dairy
The updated guidelines also reflect a more nuanced understanding of dietary fat.
Full-fat dairy products without added sugars are now included as part of a healthy dietary pattern. This marks a shift away from decades of blanket low-fat recommendations and acknowledges the importance of nutrient density, satiety, and sufficient protein intake.
For many older adults, removing fat from the diet often led to unintended consequences, including increased reliance on refined carbohydrates and reduced overall food satisfaction. The new approach recognizes that healthy fats play a role in energy balance, nutrient absorption, and overall dietary quality.
Whole Foods Over Ultra-Processed Foods
For the first time, the guidelines take a clearer stance on ultra-processed foods.
Highly processed foods are now explicitly discouraged, with a stronger emphasis on whole, minimally processed ingredients. This reflects growing evidence linking ultra-processed diets to inflammation, insulin resistance, cardiovascular disease, and cognitive decline.
Older adults may be particularly vulnerable to the negative effects of ultra-processed foods, as these products often displace more nutrient-dense options and contribute to blood sugar instability and chronic inflammation. Prioritizing whole foods supports better metabolic health and long-term function.
Blood Sugar Stability and Refined Carbohydrates
Another important shift is the stronger guidance around refined carbohydrates and added sugars.
While whole grains remain recommended, added sugars are described as unnecessary in a healthy diet. The guidelines encourage minimizing refined carbohydrates that can lead to rapid spikes in blood sugar.
Many older adults experience impaired glucose tolerance, even without a formal diagnosis of diabetes. Progressive longevity research has long shown that frequent blood sugar spikes contribute to vascular damage, inflammation, and cognitive decline. Supporting stable blood sugar is foundational to both physical and brain health.
Diet and Brain Health
Emerging research in brain aging has also shaped these updated recommendations.
Dietary patterns rich in vegetables, healthy fats, and high-quality protein have been associated with slower cognitive decline and reduced risk of neurodegenerative disease. Approaches such as the Mediterranean and MIND diets have emphasized these principles for years, particularly the importance of omega-3 fatty acids, antioxidants, and micronutrients that support neuronal health.
The guidelines’ emphasis on whole foods and nutrient density aligns closely with this growing body of cognitive longevity research.
A More Cautious View on Alcohol
Alcohol guidance has also evolved.
Rather than recommending specific daily limits, the new guidelines advise reducing alcohol consumption overall to support better health. This reflects a growing recognition that even moderate alcohol intake can negatively affect sleep quality, balance, blood pressure, and cognitive function, particularly in older adults.
Longevity research has increasingly questioned the idea that moderate alcohol consumption is protective, favoring a more individualized and cautious approach.
Longevity Science Enters the Mainstream
Many of these updates mirror principles that progressive longevity and metabolic health research has promoted for years.
Adequate protein, whole foods, healthy fats, blood sugar stability, and minimal reliance on ultra-processed foods have long been central to strategies aimed at extending healthspan rather than simply lifespan. What was once considered cutting-edge science is now reflected in national nutrition policy.
This alignment signals a broader shift toward evidence-based, function-focused approaches to aging.
What This Means at Ciela
Wellness and longevity have always been foundational to how we design our community, programs, and dining experiences.
The updated Dietary Guidelines reinforce principles that are already core to our approach: prioritizing fresh, nutrient-dense foods, offering balanced and protein-forward meals, minimizing ultra-processed ingredients, and supporting dietary patterns that promote long-term health, vitality, and quality of life.
As these guidelines shape national programs and healthcare recommendations, it is encouraging to see science-driven nutrition strategies that have long guided progressive aging and longevity research becoming part of the mainstream conversation about aging well.


.svg)